The Power of Patient Organizations in Advancing Health Equity
Exploring Initiatives That Drive Equitable Impact for Patients And Communities in the United States
Introduction
In the United States, health equity has emerged as a key idea for ensuring everyone receives the care they need, and for good reason. Inequity in healthcare is associated with an extra $320 billion in annual healthcare spending. These costs may grow to $1 trillion by 2040 unless resolved.¹ Patient advocacy organizations (‘patient organizations’) serve as important stakeholders on the journey to more equitable care as they work to bridge gaps in care and access for people with various health conditions.² Efforts of patient organizations to support, educate, and empower patients and communities who have been historically and systemically denied adequate resources and quality care can be especially powerful.
However, more clear data on how patient organizations collectively drive health equity is needed. DKI Health launched a first-of-its-kind study to measure how patient organizations think about health equity, where they have had successes, and which barriers still exist. The results of this study provided insights into impactful activities, and these findings will be relevant for life sciences companies looking to form genuine, long-lasting relationships with patient organizations to advance health equity.
Note: Throughout this report, the word “organization” will refer to patient advocacy non-profit associations and “life sciences companies” will refer to companies providing medical products and devices, including biotech, pharmaceutical, and medical device companies.
EXECUTIVE SUMMARY
Guiding Principles for Life Sciences Companies in Partnering with Patient Organizations on Health Equity
1: Maximize Impact of Support
Build trusted, transformational relationships that extend beyond financial support
Create sustainable health equity initiatives through multi-stakeholder collaborations, including healthcare providers and local community organizations
2: Enhance Structural Frameworks
Focus on intersectionality when discussing diversity, and ensure equity initiatives encompass a wide range of social determinants
Support the development of health equity strategies, informed by patient input
Offer training and education, led by experts on health equity
Share connections with diverse talent pools to enable easier access to qualified candidates
Provide data and resources to support the needs of diverse patient populations
3: Diversify Clinical Trials
Involve patient organizations (and patients) from the earliest stages of clinical development, to design and optimize trials
Connect patients with healthcare providers who can share information about clinical trials
Introduce innovative tools that make it easier for patients to enroll and participate in trials
Provide information about clinical trials in patients’ primary languages
Follow-up & maintain ongoing communications with patients and their families post-trials
Methodology
DKI Health conducted a 20-minute web-based survey with leaders from 42 patient organizations based in the United States who represent various health conditions.³ Following completion of the survey, eight survey respondents participated in a 60-minute interview to provide further insights.⁴ Additionally, three independent health equity experts provided input into the survey design, with one of whom we conducted a follow-up interview.
Key themes explored:
How patient organizations define health equity
Whether organizations have a health equity strategy in place, and if so, how well they execute these strategies
To what extent are organizations committed to diversity and inclusion, and how well do they promote it within their organization
How well organizations use data to drive health equity
How well organizations are able to impact equity in clinical trials, measuring efforts to inform and reach patients, either alone or in partnership with clinical trial sponsors
How can life sciences companies best support patient organizations in their efforts to improve health equity across patient communities
Key Insights and Recommendations
In this paper, we explore the potential for life sciences companies to advance health equity through strengthened relationships with patient organizations and share three guiding principles to support meaningful actions based on the survey and interview results.
1: Maximize Impact of Support to Patient Organizations
Build transformational relationships with patient organizations beyond just funding
While 62% of surveyed patient organizations prioritize health equity, 72% of leaders believe their organization’s focus on health equity needs improvement. Various methods can drive these improvements.
Level of priority of health equity (HE) to patient organizations
62% of patient organizations make health equity either a high or top priority. However, 72% of organizations believe they must improve their ability to advance health equity.
Patient organizations certainly welcome financial support. However, million-dollar donations are not always a requirement. Small dollar amounts that cover the cost of food at a community event, plus attendance by a company representative, can sometimes be more impactful than a large donation and no event appearances. Additionally, low-cost activities such as regular discussions, occasional visits, and sharing of existing resources can lead to significant positive change.
“A pharmaceutical representative said to me, ‘I’m going to be that guardian angel to connect you with resources’…she paid for the food, and individuals wanted to talk to her and ask questions about what was going on as far as the clinical trials [in sickle cell]. She was a hit!”
Patient advocacy leaders encourage industry sponsors to strengthen their participation in health equity-specific initiatives to increase impact and transition from being “sponsors” to being “health equity champions.”
By engaging directly with patients and communities, life sciences companies can gain a better perspective on making medical care more accessible and equitable, as 79% of patient organizations report deep engagement with local patient communities. More well-informed patients increase the likelihood of accessing appropriate medicines, improving adherence, and achieving better outcomes.⁵
“I don’t want transactional partnerships. We are leaving an impact on the table by just saying, ‘Give me some money.’ It’s not good for relationship building, it’s not sustainable, and you’re missing out on an opportunity to have a larger impact.”
Patient organizations are now expecting life sciences companies to not only fund but actively participate in successful initiatives. For example, simply having a company representative visit a patient organization and speak with patients directly fosters listening and helps build trust. Likewise, establishing a consistent point of contact at a company over time – despite staff, product, and portfolio changes – strengthens relationships.
That being said, financial support is still critical, as lack of funding is the number one barrier to implementing health equity initiatives, as cited by 90% of survey respondents. Balancing financial contributions with other resources like time and connections to medical experts can maximize the impact life sciences companies can make for patient organizations and, ultimately, patients.
“It’s frustrating when we don’t have enough funds [to conduct educational activities]. When [one company] gave us money for our patient-focused drug development (PFDD) meeting, that’s when we started learning.”
Life science companies have great opportunities to recalibrate how they distribute some of the significant funding they already provide to support patient organizations. For example, the American Cancer Society, the Leukemia & Lymphoma Society, and the National Health Council each reported receiving more than $1 million in funding from industry partners in 2022.⁶’⁷’⁸ While $1 million provides a lot of value to these organizations, innovative thinking can amplify the impact of every dollar.
“Funding for health equity [helps ensure] that equity work is sustainable and remains a priority for both patient organizations and pharmaceutical companies.”
It is also worth noting that the dollars spent on patient organizations pale in comparison to typical pharma advertising budgets – companies spent around $1.1 billion in advertising in just one month (January 2023).⁹
Companies should consider re-allocating some funds from these large marketing budgets to partner with patient organizations, who help patients learn not only about a medicine but also share a pathway for them to access all their options.
“Imagine the impact that patient organizations could have if pharma companies gave even 3% of their consumer marketing budgets to support our activities… it would be a terrific return on investment.”
Create sustainable initiatives through multi-stakeholder collaborations
Developing and implementing sustainable health equity initiatives should be a significant goal of any funding provided. Strengthening trusted relationships between life sciences companies, patient organizations, healthcare providers, and local patient and community partners such as faith-based organizations, community centers, and local businesses will lead to more significant impact.
Case Study: A New Local, Community-Based Approach for Advancing Health Equity
Physical presence is highly impactful in engaging and activating patients. Despite limited resources, patient organizations are hiring staff in local communities, aligned to areas of highest disease burden, to implement interventional activities. Dedicated staff are embedded within the community, and they collaborate with local health and other organizations. In-person interactions facilitate trust and relationship-building.
Example #1
For the past two years, during Colorectal Cancer Awareness Month, the Colorectal Cancer Alliance has partnered with corporate sponsors to improve screening rates among Black communities in Philadelphia. Shared goals included getting 5,000 Black Philadelphians screened for colorectal cancer. In a campaign called the “Spirit Challenge,” the Alliance leveraged the power of local churches to improve colorectal cancer screening rates among Black Americans, who are 20% more likely to be diagnosed with colorectal cancer, and 35% more likely to die from the disease, than non-Hispanic whites.10Bringing spiritual communities together raised awareness of the need for screening in a trusted setting; expanding the campaign to other community events, such as basketball games, increased the message’s resonance with target audiences. This successful campaign is the result of many months of discussions and trusted relationship-building among all stakeholders, including life sciences representatives.¹¹
Example #2
ZERO Prostate Cancer is committed to improving outcomes among Black populations in regions where data shows that significant health disparities disproportionately impact them. By implementing a new localized strategy, the organization is hiring staff and training volunteers in several regions, including Appalachia, Baltimore, and New Orleans, to forge strong connections with local nonprofits and create effective programs. Key goals include increasing screening rates and decreasing late diagnosis. Insights and lessons learned from these efforts will be applied as the initiative expands into additional regions. Recognizing that each local community has unique characteristics, events and activities will be designed to fit these diverse cultures, ensuring meaningful engagement with patients.¹²
2: Enhance Structural Frameworks of Patient Organizations
Focus on intersectionality
Patient advocacy leaders emphasized the importance of considering intersectionality across multiple aspects of identity when discussing diversity, equity, and/or inclusion with industry partners. They proposed including critical social determinants of health, such as socioeconomic status, geographic location, literacy levels, disabilities, and childhood adversity, in addition to race and ethnicity.
“Over 50% of the people [our organization supports] are people of color. We have programs to meet the needs of the LGBTQ+ community as well as the elderly and those that live in urban and rural areas. Often, they delay going to the doctor because they don’t have the co-pay, or they’ll delay getting radiation because they don’t have the money for gas. (Cancer patients) are facing all kinds of issues, and the top three are affording food, rent, and utilities.”
“In conditions like obesity, we tend to completely overlook key factors, such as adverse childhood events that contributed to their obesity, or the mental health support that’s required before and after surgery or treatment…it’s not easy to have people treat you differently just because you look different or you’re smaller now…”
Define health equity policies and strategies
Making health equity a strategic priority is a significant step for any organization wanting to make an impact, followed by building supporting infrastructure, addressing multiple determinants of health, eliminating racism and other forms of oppression, and partnering with communities.¹³
While the majority of surveyed patient organization leaders (62%) reported that improving health equity is a top priority for their organization, only 43% have a written health equity policy or strategy with clear goals to advance health equity and an implementation roadmap for specific initiatives. Evidence shows that having a written strategy leads to better results – 72% of leaders in organizations with a formal health equity strategy are satisfied with their health equity activities, compared to 25% of leaders of organizations without one.
“Memorializing a written health equity strategy is so important to keeping the organization on track. Whenever we do an activity to help patients, that strategy is like a North Star guiding us towards our goals.”
HEALTH EQUITY FRAMEWORK AT THE COLORECTAL CANCER ALLIANCE¹⁴
The Colorectal Cancer Alliance built a framework to visualize the key pillars necessary to advancing health equity. These include: partnerships, culturally appropriate education and support, grassroots community engagement, and funding.
Organizations who reported they were “doing well” on health equity focus more on strengthening internal structure, dedicating more funds, and engaging more in clinical trials with patients.
Operationalizing health equity strategy
Organizations who described themselves as “doing well” with advancing health equity outperformed those who described themselves as “Needs Improvement'' on all metrics. The metrics were: receive health equity funding, have a health equity department, have a health equity team, have a health equity designated role, and have a health equity strategy. Organizations that are doing well allocate more of their budget to health equity activities, and do more to advance health equity in clinical trials, including education, addressing mistrust, and connecting patients with healthcare providers (HCPs).
The majority (72%) of the organizations that have a written health equity policy or strategy reported creating their strategy with input directly from patients, while 61% consulted external experts. It is essential that those who are supposed to benefit from a policy are asked for input on that policy. Likewise, experts in the field should provide their insights. Failure to include either perspective, particularly the patients’, opens the door for a health equity strategy to contain mistakes that make it less effective.
“We need to take a step back and humble ourselves. In the medical and public health worlds, we must remember that we don’t know everything, and it’s very important that we listen to patients and to communities. And that’s where we’re going to get the most knowledge and learn the best ways to really work with them.”
Life sciences companies are well-positioned to support organizations as they define their own health equity policies and draft their strategies. By inviting independent health equity experts, offering multilingual educational resources, and facilitating connections between patient organizations and healthcare providers, companies can enhance the ability of patient organizations to develop and implement effective health equity initiatives.
Provide training, connections, and resources
Once written health equity strategies are in place, supporting the infrastructure of patient organizations to allow effective implementation is needed. These include sufficient education and training on health equity, representative staff and team members, and required data or other resources.⁹
Training and Education
Of the surveyed organizations, only 57% reported having any kind of training programs on health equity, while leaders from 71% of the organizations felt like they could be doing better on their health equity initiatives. For organizations that currently have training programs, educational content included a universal definition of health equity, historical cases and statistics demonstrating systemic inequities, social determinants of health, and strategies for effectively addressing health disparities. These sessions gave staff members the opportunity to ask difficult questions and provided a safe space for candid discussions.
Without robust training, health equity initiatives are less likely to meet their goals.¹⁵ Life sciences companies are able to connect patient organizations with experts and/or existing training programs to strengthen their educational efforts.
Staffing
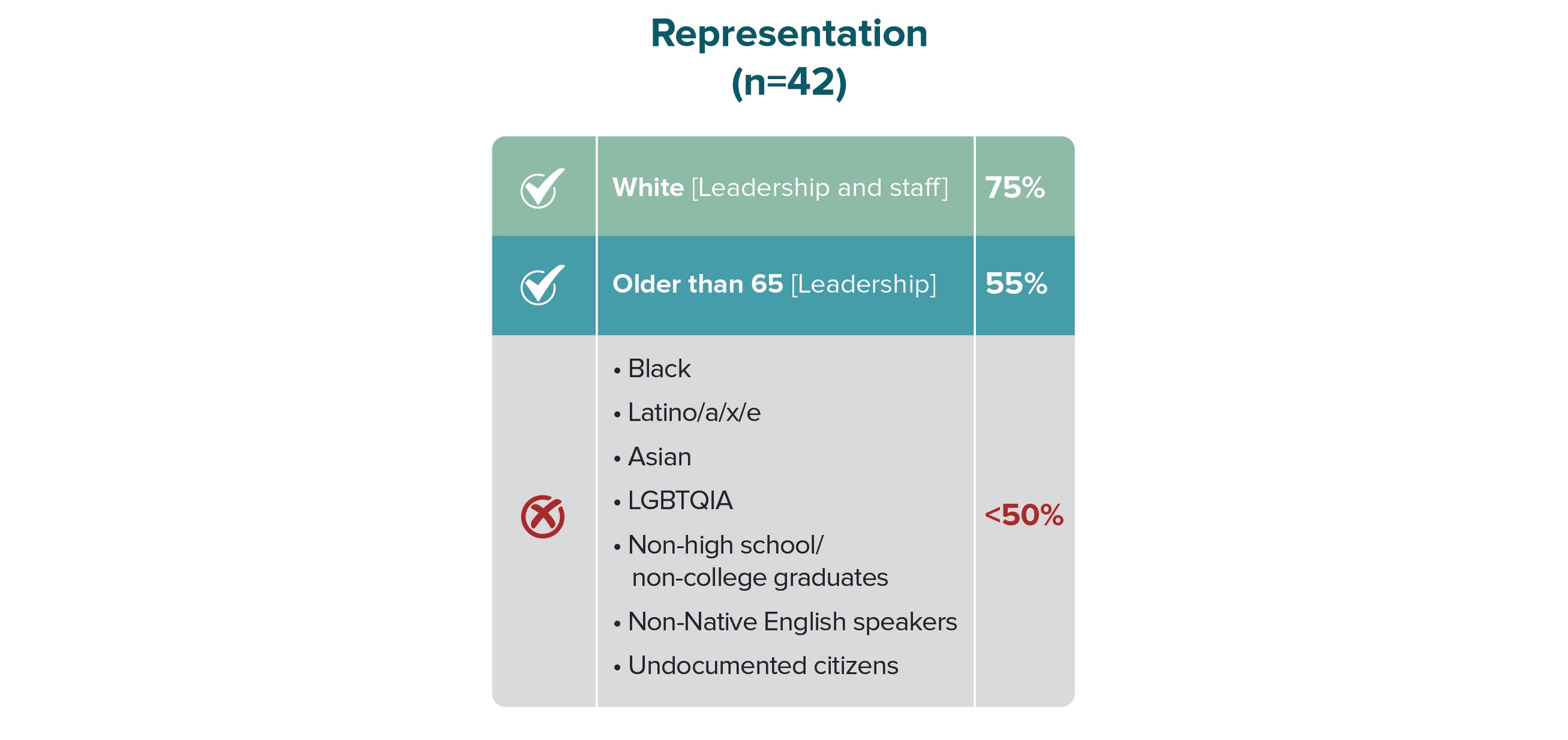
More than half (60%) of the patient organizations surveyed indicated that their leaders and advisory board members adequately represent the patient populations that the organization serves. However, this number decreased to 50% or below when asked specifically about representation related to race, ethnicity, gender, or sexual orientation.
Level of diversity within patient organizations
60% of organizations agree that the diversity of their leadership team and advisory board reflects the diversity of the patient population that they serve. 50% of organizations agree that their staff diversity is representative of the patient population that they serve. 43% agree that the diversity of sexual orientation of staff is reflective of the patient population.
Specifically, more than 75% of the organizations reported that both their leadership and staff members adequately represented White patients; while 55% reported that leadership adequately represented patients who were 65 years or older.
However, less than 50% of organizations believed that their organization adequately represented Black, Latino/a/x/e, Asian, LGBTQIA, non-high school/college graduates, non-Native English speakers, or undocumented citizens.
Limited data for Native Americans, Native Alaskans, Native Hawaiians / Pacific Islanders, and Middle Eastern / North Africans did not allow for a discrete conclusion. It is likely that these racial and ethnic groups are also underrepresented.
White people are adequately represented among staff and leadership, while those older than 65 years are adequately represented in leadership. All other patient populations surveyed are under-represented.
Despite the lower than ideal levels of diversity among patient organizations, leaders generally recognize the strong relationship between diverse staff and improvement in health equity initiatives. A persistent issue in advocacy hiring is that organizations struggle with recruiting staff members who are qualified to implement health equity initiatives. 64% of organizations reported being unable to find staff with the required lived experiences, cultural competencies, or geographic proximity to patient communities being served by the organization. Efforts to recruit diverse staff must continue, as qualified candidates exist. In the long run, having a diverse staff will lead to more impact with health equity initiatives.¹⁶ Organizations could potentially recruit from the patients they serve as lived experience is often an overlooked criterion for a qualified candidate.
“Everyone in our organization is responsible for health equity. It is embedded within our programming and is always integrated into the developmental process. We want to make sure that we have folks who can make sure we don’t forget about equity.”
Life sciences companies can support patient organization’s recruiting efforts through access to diverse candidate networks and databases. They can also foster collaborations with other advocacy, grassroots, and/or community organizations that reach the target patient populations.
“The value of having diverse staff is that each staff member is bringing their intersectional journey, interpreting health equity within that, but also being respectful of other colleagues that work in the space. I learned a lot from colleagues that belong to other racial/ethnic groups and sexualities. That is not a part of my lived experience, but it has helped me grow professionally and I think it’s important, if you sit in these roles, to be open to that constant learning.”
Data
Of the surveyed organizations, 71% collect and utilize data to help improve health equity activities. Such data includes patient demographics, social determinants of health, and data from studies/literature. Data sources include patient surveys and interviews (20%), patient registries/databases (10%), and feedback from meetings and events (10%).
“We recently implemented a patient survey to identify unmet needs. As part of this, we collected information about health equity and demographics to analyze data.”
However, the majority of organizations do not have the resources to disaggregate gathered data by either a patient’s race/ethnicity (55%) or language (74%).
“We recently conducted a prevalence study with focus on national and state demographics and social determinants of health.”
Life sciences companies can strengthen patient organizations’ health equity infrastructure development in several ways: by offering relevant training programs and educational materials, providing connections to health equity experts and diverse talent pools, and sharing existing or new data sources. Such support can also be re-packaged and shared with multiple patient organizations, as core health equity concepts can apply to many patient populations across diseases and regions.
3: Diversify Clinical Trials through Deep Engagements
Increasing diversity in clinical trials remains the most pressing health equity issue facing the life sciences industry, despite decades of discussions aimed at increasing representation in medical research.¹⁷
Patient organizations are keenly interested in learning about and getting involved in new and ongoing clinical trials sponsored by life sciences companies. For example, 55% of survey respondents reported that they learn about the latest clinical trials from healthcare providers (HCPs); 54% educate their patients about new clinical trials; and 39% connect patients to HCPs who will help them enroll in clinical trials.
“On a quarterly basis, we pull all the trials on clinical trials.gov and upload them to our website, so they are accessible [to our patients]. Then [people] can search by where they live to see if there’s a clinical trial in that area. We’ve been thinking more and more about the amount of money we invest in maintaining that clinical trials database. We’re trying to figure out a way to continue funding it [because it is important]. ”
Despite this high level of interest, patient organizations are generally not made aware of clinical trials by industry sponsors. When asked whether various pharmaceutical companies provided information about relevant clinical trials to patient organizations, almost 70% said never. Even among companies who were mentioned as sharing information about clinical trials either “always” or “frequently” by at least one organization, less than 20% of the remaining organizations agreed, despite reporting good relationships.*
*Companies evaluated included Abbvie, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Gilead, GSK, Johnson & Johnson, Lilly, Merck & Co, Novartis, Novo Nordisk, Pfizer, Roche/ Genentech, Sanofi, Takeda.
Pharma companies making patient organizations aware of current clinical trails
Only a few patient organizations are made aware of clinical trials by most surveyed companies. Most patient organizations are not made aware of clinical trials by any company.
Even for organizations made aware of clinical trials, significant pain points exist for patients' participation in clinical trials. Patient organizations continue to be frustrated by requests from clinical trial sponsors to support recruitment for protocols that are poorly designed or that unintentionally prevent diverse patients from participating.
Some life science companies’ approach of paying for clinical trial promotions within patient organizations do not feel authentic, undermining trust and collaboration.
“We have been offered $15,000 by a pharmaceutical company to promote their clinical trial. Firstly, that’s no longer the transactional way for us to do business. Those partners would like us to run ads because patients want to hear from a trusted nonprofit. Secondly, our name, brand, and credibility is worth more than $15,000. You know, part of the reason why sometimes we have to help recruit diverse patients is because they haven’t designed their trials properly. I want us to be much more involved on the front end, so they’re not sitting there going, ‘Oh, well, we’re really trying to, you know, recruit people of color.’ I’m like, ‘Great, but your exclusion criteria is so stringent that you are automatically [excluding them].’ I want to have much more of a conversation of ‘Oh, if you’re having a challenge recruiting, let’s help you get to the root of why that is – not just like ‘Hey, pay us money, and we’re going to put out some social media.”
Other barriers to improving equity in clinical trials persist. The top five reasons patients do not participate in clinical trials, as reported by survey participants, included the following:
Patients are fearful of clinical trials and unknown outcomes (57%)
Patients are not aware of clinical trials (55%)
Patients do not trust the healthcare system and/or the clinical trial process (48%)
Patients do not have the financial resources required to participate (45%)
Patients do not have a caregiver or family member to assist in care (38%)
Most common barriers to helping patients participate in clinical trials
The most common barriers patients face in participating in clinical trials include: fear/uncertainty, lack of awareness, mistrust, lack of financial resources, and lack of caregiver or family support.
For patients who participate in clinical trials, a general lack of follow-up by the clinical trial sponsors continues to cause frustration. Patients want to know what the results are to know if the drug is successful or not because of the risks they are taking. Even if a trial fails, patients desire to know the outcomes.
“Patients are asking for clear communication about what’s going on, what their situation is, what the prognosis is. And then if they do participate in a trial, a lot of patients that I’ve spoken to recently said they participated in a trial, and they never heard anything [about the results]. Which really has them [angry], you know, that’s a no, no.”
Life sciences companies can improve diversity in clinical trials, enhancing health equity, by seeing patients and integrating patient organizations as key partners in the drug development process. An easy win is to share information about new and upcoming clinical trials with all relevant patient organizations. Considering that 22% of US residents speak a language other than English at home,¹⁸ providing information about clinical trials in multiple languages will be critical.
For a deeper, more long-term impact, companies should involve patient organizations in clinical study design and protocol development from the early stages of drug development. This will ensure that protocols are developed with patient input and that inclusion criteria are broad enough to allow diverse patient groups to participate. This will also help strengthen long-term, transformational relationships with patient organizations.
“Pharma needs to engage patient organizations and patients earlier. Companies have said to me, ‘We wish we had done this two years ago, we would have saved a lot of grief and would have been better equipped had we started working with you [on clinical trials] earlier.’ ”
To address the general mistrust of the biopharmaceutical industry, it is essential for companies to empower not only patient organizations but also trusted healthcare providers such as physicians, nurses, pharmacists, public health professionals, and community health workers. Patients are much more likely to act upon information from HCPs they have known for years and talk to frequently.¹⁹ Companies that convince HCPs that a clinical trial will benefit their patients will have an easier time with recruitment. HCPs serve as trusted messengers who can effectively communicate clinical trial information to patient communities, fostering confidence and transparency.
“Obesity is complex. This pharmaceutical company [we are working with] is in early stages of development, but it is smart enough to know that they can’t wait until Phase III to [bring us in].”
Lastly, companies must consider new and innovative methods for efficient clinical trial recruitment. Using digital tools such as mobile phone apps can help patients enroll and participate in trials.²⁰ When possible, allowing patients to be treated at a local clinic or even receive treatments at home can gather more inclusive data and enable more people to participate in research.
Conclusion
Patient organizations are essential partners in advancing health equity. For life sciences companies, building long-term and trusted relationships with them must reflect respect for the organization’s expertise in serving patients. Blending financial support with collaborative, multi-stakeholder engagements is crucial for driving sustainable change in health equity.
For Further Research
This study assessed current perceptions and practices regarding health equity among 42 U.S.-based patient organizations, 29% of which are located in the Washington DC area. Future research could benefit from including a broader array of organizations that vary in size, focus, and geographic distribution. Additionally, conducting a follow-up study on a global scale to explore how health equity is defined and advanced outside of the U.S. could provide further insights to inform effective strategies.
References
Robeznieks, A. (2023, June 19). Inequity damages health-and drains the economy. American Medical Association. https://www.ama-assn.org/delivering-care/health-equity/inequity-damages-health-and-drains-economy#:~:text=Achieving%20optimal%20health%20for%20all&text=The%20Deloitte%20Health%20Equity%20Institute%20report%20says%20health%20inequities%20account,and%20%242.4%20billion%20treating%20asthma.
National Health Council, 2018. https://nationalhealthcouncil.org/blog/the-benefits-of-nhc-membership/. Accessed April 12, 2024.
DKI Health fielded the web-based survey with 42 patient organizations between August 2023-February 2024, representing many health conditions including cancer, cardiovascular, gastrointestinal, infectious, neurological, obesity, rare, respiratory, sickle cell, women’s health, and surgeries.
DKI Health conducted interviews with 8 select patient organization leaders in March 2024.
Nutbeam, D., & Lloyd, J. E. (2020, October 9). Health Literacy in Primary Care Practice. Understanding and Responding to Health Literacy as a Social Determinant of Health. https://nursing.jhu.edu/wp-content/uploads/2023/02/Health-Literacy-in-Primary-Care-Practice.pdf. Accessed April 12, 2024.
American Cancer Society, 2022 Annual Report, https://www.cancer.org/content/dam/cancer-org/online-documents/en/pdf/reports/2021-2022-annual-report-2.pdf. Accessed April 12, 2024.
Leukemia & Lymphoma Society, 2022 Annual Report, https://llsorg.widen.net/s/wqpgcmfwm9/lls-annual-report-2022. Accessed April 12, 2024.
National Health Council, Business and Industry Sponsors, https://nationalhealthcouncil.org/members/?m_cat=74&m_key=. Accessed April 12, 2024.
Statista. Pharma advertising spending in the United States from October 2022 to January 2023. https://www.statista.com/statistics/1407234/pharma-ad-spend-us/. Accessed April 12, 2024.
Colorectal Cancer Alliance, https://colorectalcancer.org/about-us/our-impact/alliant/alliant-december-2022. Accessed April 12, 2024.
CBS News, Philadelphia churches raise awareness for colon cancer screenings while competing in Spirit Challenge, March 18, 2024. https://www.cbsnews.com/philadelphia/news/philadelphia-colorectal-cancer-alliance-spirit-challenge/. Accessed April 12, 2024.
Interview with Zero Prostate Cancer. March 2024.
Institute for Healthcare Improvement, Improving Health Equity: Make Health Equity a Strategic Priority: Guidance for Healthcare Organizations. 2019. https://www.chausa.org/docs/default-source/health-equity/1_ihi_improvinghealthequity_makeequitystrategicpriorityguide.pdf. Accessed April 12, 2024.
Colorectal Cancer Alliance, https://colorectalcancer.org/about-us/diversity-equity-and-inclusion-alliance. Accessed April 18, 2024.
Skorton, D. J. (2020, October 8). How diversity training for health care workers can save patients’ lives. USA Today. https://www.usatoday.com/story/opinion/2020/10/07/why-diversity-training-medical-schools-can-save-patients-lives-column/3635406001/
Zephyrin, L. C., Rodriguez, J., & Rosenbaum, S. (2023, July 20). The case for diversity in the health professions remains powerful. Commonwealth Fund. https://www.commonwealthfund.org/blog/2023/case-diversity-health-professions-remains-powerful
Food and Drug Administration. Enhancing the Diversity of Clinical Trial Populations — Eligibility Criteria, Enrollment Practices, and Trial Designs Guidance for Industry. Nov 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enhancing-diversity-clinical-trial-populations-eligibility-criteria-enrollment-practices-and-trial.
The United States is rich in languages. https://share.america.gov/united-states-rich-in-languages/. Accessed April 12, 2024.
Arditi, L. (2023, December 22). More patients are losing their doctors – and their trust in the Primary Care System. NPR. https://www.npr.org/sections/health-shots/2023/12/22/1221043147/more-patients-are-losing-their-doctors-and-their-trust-in-the-primary-care-syste
McNamara D. Decentralized clinical trials could boost diversity in research. Miller School of Medicine, University of Miami. December 15, 2023. https://news.med.miami.edu/mobile-app-boosts-clinical-trial-diversity/. Accessed April 12, 2024.
Acknowledgements
DKI Health would like to thank our Advisors who guided us on the need for this survey, provided input into the survey design, and reviewed the recommendations.
Advisors
April Avilés, Racial Equity and Public Health Leader
Courtney Bugler, CEO and President, Zero Prostate Cancer
Phil Gattone, CEO, National Bleeding Disorders Foundation
Jen Grand-Lejano, American Cancer Society Cancer Action Network
Mary Kemp, Advocate, American Cancer Society Cancer Action Network
Sue Koob, CEO, Preventive Cardiovascular Nurses Association
Alisha Lewis, Founder and CEO, Genèsic Health
Joe Nadglowski, President & CEO, Obesity Action Coalition
Christian Lillis, Co-Founder and CEO, Peggy Lillis Foundation
Arya Singh, Advocate and Author
Sharon Washington, Diversity, Equity and Anti-Bias Consultant
We would also like to thank the patient organizations who participated in the survey and interviews.
Participating Organizations
American Lung Association
AXYS
Bone Health and Osteoporosis Foundation
CancerCare
Colorectal Cancer Alliance
Genèsic Nonprofit Organization
GRIN2B Foundation
Hepatitis B Foundation
Indo Us Organization of Rare Diseases
International Pemphigus & Pemphigoid Foundation
international Sacral Agenesis/Caudal Regression Association
Lowe Syndrome Association
Lung Transplant Foundation
Marked By Covid
National Health Council
National Menopause Foundation
Our Odyssey
Peggy Lillis Foundation
Pheo Para Alliance
Progressive Familial Intrahepatic Cholestasis Advocacy and Resource Network
Sepsis Alliance
Spina Bifida Association
Superficial Siderosis Research Alliance
Superior Mesenteric Artery Syndrome Research Awareness and Support
SYNGAP1 Foundation
The Alliance to Cure Cavernous Malformation
The Leukemia & Lymphoma Society
VHL Alliance
ZERO Prostate Cancer
+ 13 organizations who prefer to remain anonymous
Survey Execution
This study was made possible with support from Nick Lapolla and Mike Moyer at MedSurvey.
Funding
This project was funded by DKI Health. All participants were compensated.
Authors
Deepa Dahal, Co-Founder & Executive Partner
A global citizen who embraces her intersectional identity to create a world where good health is possible, accessible, and equitable.
Nolan Gibson, Manager
An innovative thinker who is passionate about turning unmet needs into actionable insights and improved patient outcomes.
Casandra Kennedy, Consultant
A public health enthusiast who enjoys collaborating with diverse stakeholders to improve the health of communities worldwide.
Alysha Ebrahim, Consultant
A changemaker who is committed to advancing equitable healthcare by designing affordable and accessible solutions.